2.6 mins read | Physical Therapy Rehab
Women’s Health Rehab: Piles
Written by Anamika Bheda, Maria Dalal
Graphics by Nimisha More
Visual Media by Param Sampat
Audio by Aparna Premraj
Share this article
Peek into
Too Bored to watch the entire video? We have got you covered! Listen to the full Interview on the go –
What are hemorrhoids? Nothing but the veins at the lower part of the rectum and anus that act as cushioning and are the cost of our erect posture! When these vein walls are stretched thin or irritated, they become painful, swollen, and bulging.
Over 4.4% of the general population have piles, and the peak incidence is between 45 to 65 years of age. [1] Men are more likely to seek treatment than women.
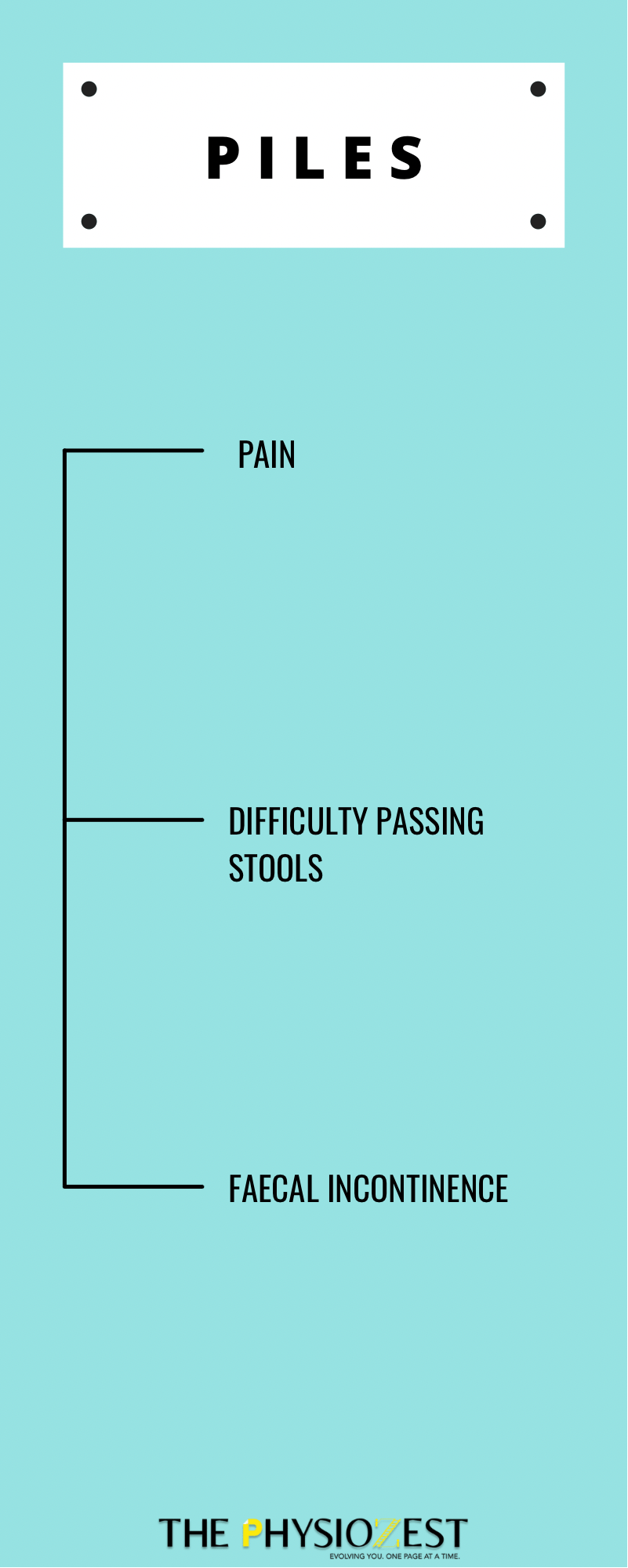
The symptoms of Piles can range from mildly irritating to debilitating. They can present as
If the causes are not addressed, it can also lead to fecal and flatus incontinence.
The causes of this common but complex condition are multifold.
Also Read: Paralympics: A Panel Discussion
How can Exercise help?
To address symptoms:
1. Pain – Cryotherapy

2. Difficulty Passing Stools – Pelvic floor Relaxation. Breath Coordination, Core Strengthening and TA bracing

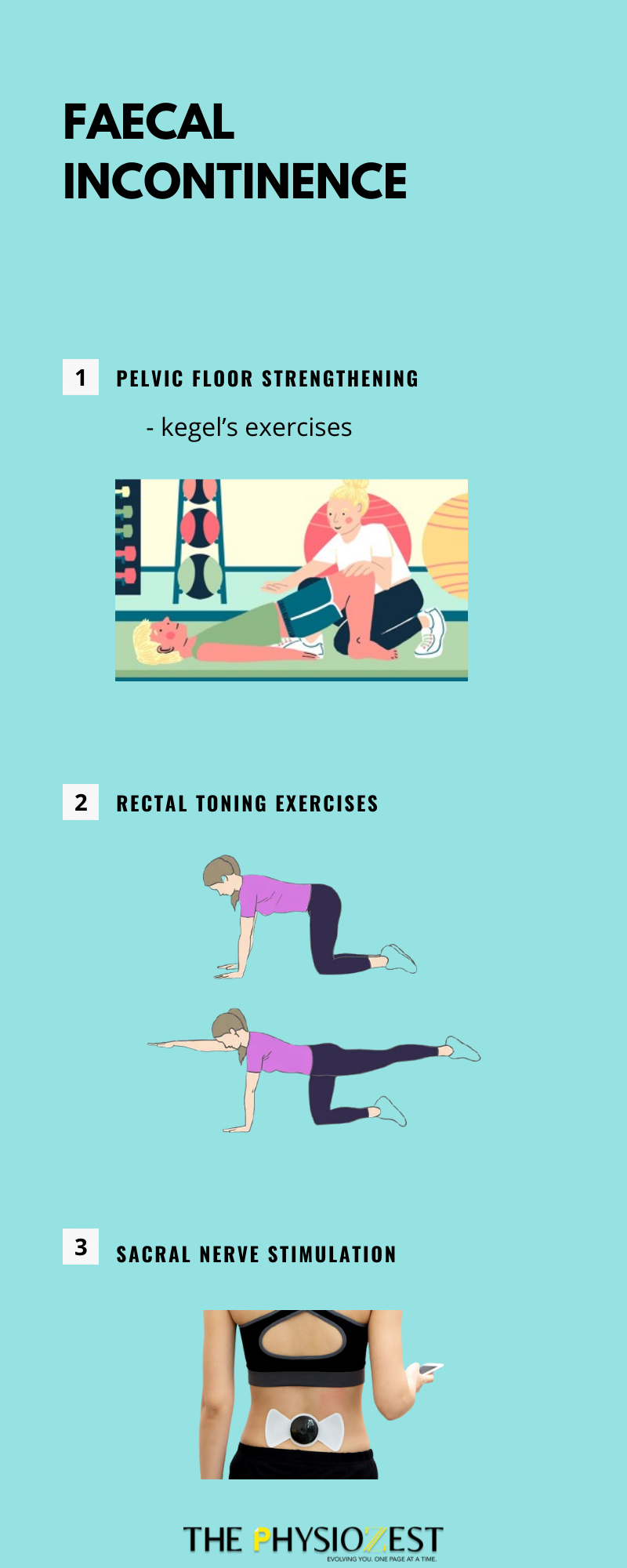
3. Fecal flatus incontinence – Recal toning, Sacral Nerve Electrical Stimulation
4. To address the etiology
5. Lifestyle Modifications
The dysfunction of the pelvic floor (the layer of muscles that support our abdominal organs like a sling), can arise from 3 means:
Kegels without PF relaxation is incomplete training- like heel raises on stilettos.