7 Clinical Tips While Treating an OA Knee case: Let’s treat those cracking knees
Written by Nirja Shah
Graphics by Ria Gorey
Share this article
Did you know that osteoarthritis affects 302 million people worldwide and is the leading cause of disability in the elderly? It lasts for decades in the life of a patient.
There are currently no established disease-modifying interventions that can prevent or reverse OA-related cartilage loss or disease progression. As a result, treatment focuses on relieving pain while also maintaining or improving physical and psychological function. Rehabilitation has hence become the primary point of treatment for OA knee. Clinicians can use the recommendations mentioned below to help them choose among the available treatments that have been shown to produce the best results possible.
1. Tell Them just the right things!
Rather than discussing the pathophysiology of the disease, focus on informing patients about their joint pain and the risk factors they should be aware of. This reinforces to the patient that clinical management aims to deal with pain and its consequences, rather than instilling fear/anxiety about “joint damage” or the possibility of the condition worsening with continued joint use. “Joint pain” emphasizes the issue without conjuring up images of a hopeless structural problem that can only be alleviated through surgery. Patients need to be educated on the disease (signs, symptoms, and risk factors) and the effects of their medications, and any side effects. Educate them on joint protection measures and fitness and exercise goals and approaches to strengthen their knowledge and take action to change their behavior regarding physical activity and exercise.[1].
2. Keep Chanting “You’ve Got This!”
Several studies have highlighted the effects of self-efficacy and self-management. A passive coping style, in which people become behaviorally inhibited and avoid taking an active role in self-management of their pain, has been consistently linked to poorer outcomes. Studies show that when Individual goal setting is highlighted, that is when their own decisions drive the patient, the chance of success is more realistic[1]
Therapists should create a multidisciplinary group-based program that combines sessions on developing their skills by setting specific goals and resolving any problems that may arise, all while employing a positive thinking approach.
3. Tailor The Exercise For Each Patient
We have always been trained to seek the “best” exercise and the optimal dosage (duration, intensity, and frequency); however, current evidence is insufficient to recommend specific exercise prescriptions. Instead, exercise recommendations to patients should be based on their preferences and access. Assume a patient does not find a particular type of exercise acceptable for various reasons, including their background, upbringing, or other personal factors. In that instance, recommending that activity is unlikely to be effective; instead, the therapist should adjust the exercise to achieve the same result. When developing a program for a patient, therapists must keep in mind that some activities may be more difficult than others, and patients may try to avoid them. It is then your obligation to emphasize the benefits and keep the patient motivated to complete them. Based on the available literature, the following types of exercise may benefit the patient based on access:
- Aerobic exercise- either on a treadmill or as supervised, community-based, indoor walking.
- Strengthening exercise- isokinetic weight machines, resistance exercise training with and without elastic bands, and isometric exercise.
- Neuromuscular training- series of dynamic maneuvers of increased complexity.
- Aquatic training can also aid with components of cardiovascular fitness and activities for improving joint range of motion in a low-impact environment.
Kraus et al. assessed the impact of physical exercise on knee and hip osteoarthritis in a systematic umbrella review. They concluded that physical activity, regardless of mode, reduces pain, improves physical function, and enhances the quality of life.
4. Losing A Few Pounds Never Hurt Anyone
There is a dose-response relationship between the amount of weight loss and symptom or functional improvement in patients with OA
Did you know??
Obesity combined with OA not only impairs the knee’s load bearing abilities, but also increases the joint’s susceptibility to pain due to increased leptin accumulation in the cartilage. Furthermore, it has a variety of psychosocial effects such as negative eating behaviour, increased injury risk, and poor stress responses, all of which contribute to the development of chronic pain and cardiovascular co-morbidities..
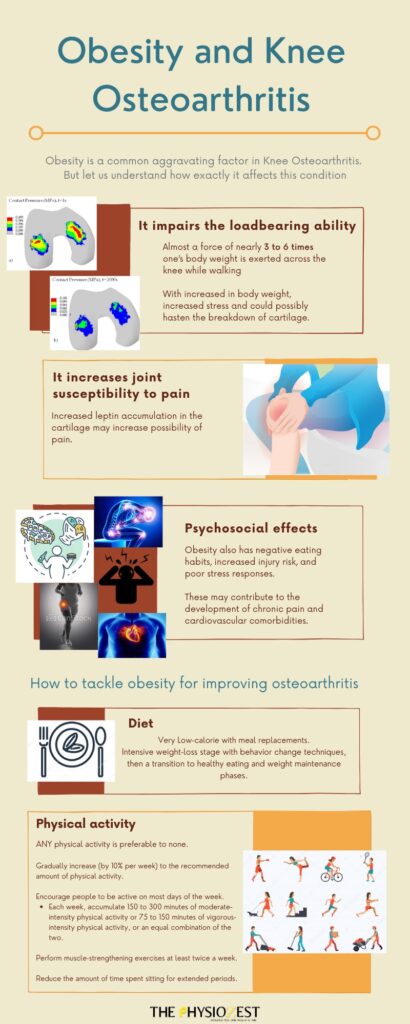
A ≥ 5% weight loss is associated with changes in clinical outcomes.
Typically, instruct the patient to follow a very low-calorie diet that includes meal replacements. In general, an intensive weight-loss stage that includes behavior change techniques is followed by a transition to healthy eating and weight maintenance phases. The goal is that behavior change skills introduced at the start of a program will assist individuals in adopting sustainable lifestyle changes conducive to long-term weight loss maintenance.
Any physical activity is preferable to none. If your patient currently does not engage in any physical activity, begin by encouraging them to do so and gradually increasing (by 10% per week) to the recommended amount. Encourage people to be active on most, if not all, days of the week. Each week, accumulate 150 to 300 minutes of moderate-intensity physical activity or 75 to 150 minutes of vigorous-intensity physical activity, or an equivalent combination of the two. Perform muscle-strengthening exercises at least twice a week. Reduce the amount of time spent sitting for extended periods and break up long periods of sitting as often as possible.[2].
5. Mind-Body Connection
Tai chi is highly recommended for patients suffering from knee OA. Tai chi is a traditional Chinese mind-body practice incorporating meditation, slow, gentle, graceful movements, deep diaphragmatic breathing, and relaxation. Strength, balance, and fall prevention, as well as depression and self-efficacy. Although there is limited evidence on the benefits of yoga, several studies have found positive results.[4]
6. Fewer Modalities, More Exercise
Modalities and thermal interventions are only recommended on a case-by-case basis for patients with knee OA. Recent research suggests that modalities such as diathermy and ultrasound are bogus. Because the benefits of these modalities are only temporary, they should always be combined with active exercise. Because of the equivocal results regarding the use of TENS for pain reduction in knee OA, modalities like TENS should be avoided for these patients. TENS and a sham TENS operation had no statistically meaningful difference in pain, according to research.[4-7]
7. Support those knees
Therapists should prescribe assistive devices and braces for safer ambulation. A tibiofemoral brace is strongly advised, and a patellofemoral brace is only advised on a case-by-case basis.[4]
Unloader braces (tibiofemoral brace) have recently been developed and prescribed as a conservative and postoperative treatment for OA to reduce knee pain. They lessen the varus alignment and thus the load on the medial compartment of the knee. The brace also has the effect of increasing knee joint space in the medial compartment.[8-10] Patellofemoral braces are only recommended if the osteoarthritis is in the patellofemoral compartment of the knee, as these patients are more likely to have difficulty getting into a deep knee bend. The pressure between the back of the kneecap and the rest of the joint rises dramatically as their knee bends these braces hence help decrease the knee pain.[11]
Cane use is strongly recommended in patients with knee OA who have disease in one or more joints that significantly impact ambulation and joint stability.

These Clinical guidelines aim to implement the latest evidence-based treatment techniques and ensure that all patients with OA are offered the most appropriate and effective treatment options available at any given time for increased satisfaction and improved quality of life.
References
- Holm, Inger et al. “The Active with OsteoArthritis (AktivA) Physiotherapy Implementation Model: A Patient Education, Supervised Exercise and Self-Management Program for Patients with Mild to Moderate Osteoarthritis of the Knee or Hip Joint. A National Register Study with a Two-Year Follow-Up.” Journal of clinical medicine vol. 9,10 3112. 26 Sep. 2020, doi:10.3390/jcm9103112
- Gov.au. [cited 2021 Aug 11]. Available from: https://www.health.gov.au/health-topics/physical-activity-and-exercise/physical-activity-and-exercise-guidelines-for-all-australians?utm_source=health.gov.au&utm_medium=callout-auto-custom&utm_campaign=digital_transformation
- Thijssen E, van Caam A, van der Kraan PM. Obesity and osteoarthritis, more than just wear and tear: pivotal roles for inflamed adipose tissue and dyslipidemia in obesity-induced osteoarthritis. Rheumatology (Oxford). 2015;54(4):588–600.
- Kolasinski, Sharon L., et al. “2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee.” Arthritis care & research 72.2 (2020): 149–162. Print.
- Bannuru, R. R. et al. “OARSI Guidelines for the Non-Surgical Management of Knee, Hip, and Polyarticular Osteoarthritis.” Osteoarthritis and cartilage 27.11 (2019): 1578–1589. Print.
- Sajadi, Simin et al. “Randomized clinical trial comparing of transcranial direct current stimulation (tDCS) and transcutaneous electrical nerve stimulation (TENS) in knee osteoarthritis.” Neurophysiologie clinique = Clinical neurophysiology vol. 50,5 (2020): 367-374. doi:10.1016/j.neucli.2020.08.005
- Zeng, C et al. “Electrical stimulation for pain relief in knee osteoarthritis: systematic review and network meta-analysis.” Osteoarthritis and cartilage vol. 23,2 (2015): 189-202. doi:10.1016/j.joca.2014.11.014
- Rodriguez-Merchan, E Carlos, and Hortensia De La Corte-Rodriguez. “The role of orthoses in knee osteoarthritis.” Hospital practice (1995) vol. 47,1 (2019): 1-5. doi:10.1080/21548331.2018.1527168
- Dessinger, Garett M et al. “Can an OA Knee Brace Effectively Offload the Medial Condyle? An In Vivo Fluoroscopic Study.” The Journal of arthroplasty vol. 36,4 (2021): 1455-1461. doi:10.1016/j.arth.2020.10.044
- Khosravi, Mobina et al. “An evaluation of the use of a lateral wedged insole and a valgus knee brace in combination in subjects with medial compartment knee osteoarthritis (OA).” Assistive technology: the official journal of RESNA vol. 33,2 (2021): 87-94. doi:10.1080/10400435.2019.1595788
- Callaghan MJ, Parkes MJ, Hutchinson CE, et al. A randomized trial of a brace for patellofemoral osteoarthritis targeting knee pain and bone marrow lesionsAnnals of the Rheumatic Diseases 2015;74:1164-1170.
- Rice, David et al. “Best Evidence Rehabilitation for Chronic Pain Part 5: Osteoarthritis.” Journal of clinical medicine 8.11 (2019): 1769. Print.
- Kraus V.B., Sprow K., Powell K.E., Buchner D., Bloodgood B., Piercy K., George S.M., Kraus W.E., Physical Activity Guidelines Advisory Committee Effects of Physical Activity in Knee and Hip Osteoarthritis: A Systematic Umbrella Review. Med. Sci. Sports Exerc. 2019;51:1324–1339. doi: 10.1249/MSS.0000000000001944
Contributors

NIRJA SHAH
Research & Content Writing Team

RIA GOREY
Multimedia Team