10 min read | Physical Therapy rehab
Sex Education for PT
Written by Juwayriah Dalvi
Graphics by Nidhi Joshi
Share this article
Peek into:
The sweaty bodies tangled in the act of love. The racing heart. The adrenaline high, dopamine rush. The height of need and the inevitable climax of ecstasy. Oh! What a wonder the holy act of making love! How immense is this sin of satisfaction!
Imagine – something hinders this process! Just imagine the amount of loss if someone loses the ability to have this experience or is indisposed enough to ruin the quality of it! How magnificent is this loss? How grave is this issue!
Yet, in our culture and hence by extension our work culture – sex is still taboo. The hush around the subject is so deep that the syllabus doesn’t cover it as a separate topic, the teachers do not include it in the management training process, the patients do not share their concerns regarding it and the therapists are clueless about even bringing up the subject and offering solutions if at all the subject is brought up.
Tell me honestly, can we say we have achieved full functional rehab if our patients cannot have safe sex (in a totally different context here).
When do I focus on sexual rehabilitation?
The answer is – ALWAYS. The very first aspect of management is patient education. Don’t we educate them about the precautions and contraindications regarding their ADLs? As rehab experts, it is our responsibility to understand this aspect of our patient’s life and educate them regarding the same. Almost all conditions that we manage need this aspect to be considered.
The BIGGEST pitfall!
The biggest pitfall that can be found in each and every research article that deals with sexual function is that not just in India but all over the world, more than 80% of clinicians – not just physical therapists but also physicians, surgeons, nurses – never really bring up the topic.
Many, many conditions that are managed by us require us to look at the sexual aspect of it. We have just tried to sensitize you on this topic. Although please remember – this pandora’s box has now just been opened! There is a long way to go….
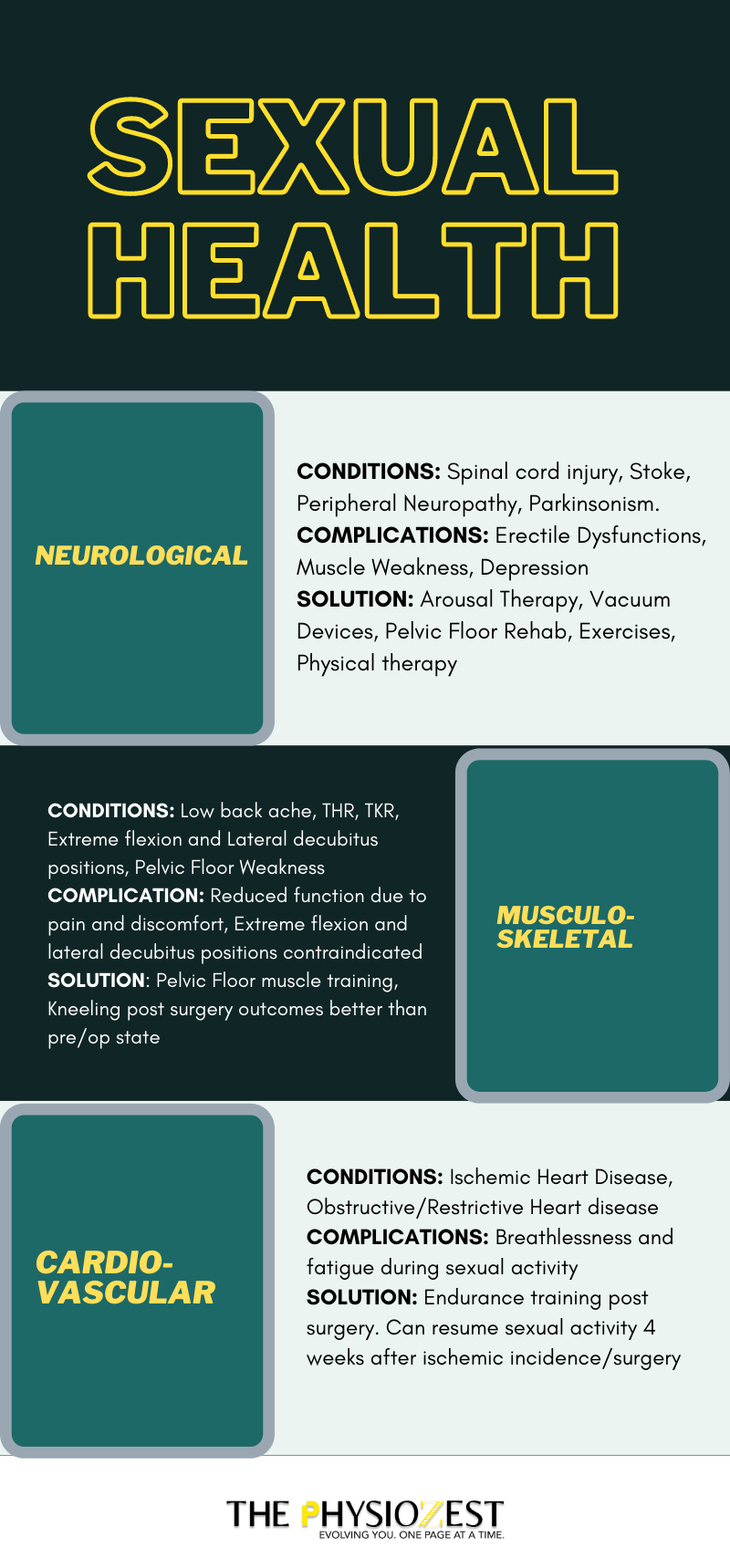
NEUROLOGICAL
| CONDITIONS | SEX-RELATED COMPLICATIONS | SOLUTIONS |
|---|---|---|
| Spinal Cord Injury /Transverse myelitis/ Cord compression [1,2] | Erectile dysfunction, self-image issues due to non-fulfilment of typical masculine norms, depression, ejaculation disorders, absence of physical arousal | Cognitive behaviour therapy, working on psychogenic arousal/reflexive arousal, specialized vacuum devices, pelvic floor rehabilitation |
| Stroke [3] | Muscle weakness, aphasia, sudden rise in blood pressure, depression, arousal dysfunction | Tailor made solutions targeting specific problems following the biopsychosocial model |
| Peripheral Neuropathies [4,5] | Sexual dysfunction (SD)*, Testesterone deficiency, muscle weakness, loss of motor control, sensory loss in limbs, discomfort due to pain and paraesthesia | Alternate/modified methods to maintain sexual function specific to the patient’s impairments |
| Parkinson’s disease [6] | Along with SD, tremor, hypomimia, muscle rigidity, bradykinesia, difficulty in fine motor control, dyskinesias, hypersalivation and sweating may interfere with sexual function. Reluctance to perform sex is also a concern | Management of the signs and symptoms with dopamine as well as exercise with good patient education and counselling can improve quality of life |
MUSCULOSKELETAL
| CONDITIONS | SEX-RELATED COMPLICATIONS | SOLUTIONS |
|---|---|---|
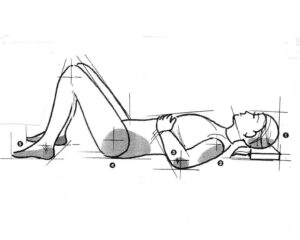
| Low Back Pain [7] | Reduction in frequency of sexual activity due to pain, discomfort, fatigue. If associated with depression and kinesiophobia — might lead to refraining from sex | Educate patients about choosing sexual positions, discuss alternate sexual activities to maintain quality of life |
| Total Hip Arthroplasty [8] | Precautions for 1-2 months, Extreme flexion and lateral decubitus position contraindicated | Research-based safe positions for both men and women |
| Total Knee Replacement [9] | 2.4 months for resuming sexual activity | Kneeling may also be possible during sexual activity post-surgery, outcomes can be better than pre-op conditions over time |
| Arthritis [10] | Difficulty in assuming sexual positions due to pain Early fatigue leading to dissatisfying sex and a reduction in sexual motivation | Most patients expressed the need of sexual counselling Working on endurance, joint pain and muscle strength |
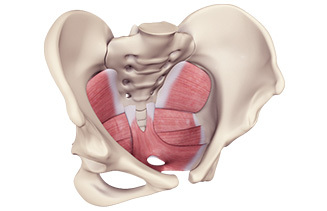
| Pelvic Floor Weakness [11,12,13] | Erectile Dysfunction, pelvic pain, reduced sexual arousal, infrequent orgasm, dyspareunia | Pelvic floor muscle training |
CARDIORESPIRATORY
| CONDITIONS | SEX-RELATED COMPLICATIONS | SOLUTIONS |
|---|---|---|
| Ischemic Heart Disease /CABG [14] | Limitations to physical activity | Can resume sexual activity 4 weeks after ischemic incidence/surgery as rehabilitation program allows that level of physical activity |
| Obstructive/Restrictive Airway Disease [15] | Reduced/no sexual activity, affected rhythm/frequency of sex, erectile dysfunction, inability to use certain positions, breathlessness and fatigue, use of bronchodilator during sexual activity | Counseling, tailor made modifications to improve sex-related quality of life in terms of positions, endurance, expected problems |
*SD (loss of genital sensitivity, erectile dysfunction, loss of vaginal lubrication, ejaculation disorder, and orgasmic disorder[4])
Although there is a lot of research that does exist on sexual function. Most of it covers the section of heterosexual vaginal intercourse. There is little literature on the other aspects of sexual activity and almost absent research for homosexuals. As clinicians, we have the obligation to be aware of the needs of all sorts of populations and their requirements. Only then we would be able to counsel them and improve their quality of life.
How do I bring up the topic?
One of the biggest challenges we will face in the Indian set-up if/when we start addressing this aspect would be – how to bring up the subject? Not saying that this process is a common occurrence even in the West. But if the West is shy – imagine us! Here are a few tips:
Of course, it sounds simple in print and would require great communication skills and presence of mind. But more than that – it would require knowledge.
What to say after I have brought up the topic?
Sex is varied. It is different for each person, each couple. To actually guide your patients in their sex life you need to know what exactly might happen during it. You yourself need to be aware of the mechanics and biomechanics of the act in detail. The varied positions, the conventional and unconventional methods, the possible scenarios, foreplay activities and the physiological impact.
It is possible that adrenaline may mask pain and discomfort and arousal might hinder judgement and caution. In such a situation, if your patient is equipped with the deep knowledge of the Do’s and Don’ts it will go a long way. We may also need to train their body structures to suit their sexual needs by exercise prescription.
If they do not seek information and we do not volunteer it – they will either having sex too soon or not at all. Both of them affect the physical recovery and/or quality of life of the patient.
Sex is as much about the mind as it is about the body….
The four stages of the sexual response cycle are – Desire, Arousal, Orgasm and Resolution. Nowhere in this cycle is there any focus on the act. As physical therapists, our domain may be to simply ensure that the physical aspect i.e. the act can go smoothly. However, we cannot achieve any of this without counseling regarding the mental process behind it. The way we are dealing with kinesiophobia and similar other psychological domains in various conditions that affect our outcomes – we also need to acknowledge that the psychosocial domain would play a role here as well.
The performance pressure, lack of desire due to pain/discomfort/side effects of medicines, the fear avoidance of movement, post trauma stress, body image deficits, behavioural and personality issues might all affect the willingness to try or lead to continual failure in sexual rehabilitation.
As physios, we can educate our patients about the expected problems and their possible solutions. We can counsel their partners or refer them to a clinical psychologist if required. But if we don’t deal with the mind, none of our efforts are going to show results.
The solution
The solution is simple yet complex. The literature has definitely picked this topic time and again. But it is scanty. As we have already seen, the solutions vary from person to person and condition to condition. But the big picture solution is pretty simple –
Sensitize the physiotherapists to address this issue
↓
Remove the prevalent stigma around it
↓
Ensure that you know what to convey/prescribe
↓
Bring a drastic change in the sex life of your patients
However, accomplishing each of these steps is a huge task. We know what to do now. We may also know how to do it. But it doesn’t make it any easier. It requires an open mind and loads of courage. A lot of – going an extra mile – to understand sex and the mechanics of it. It requires creativity and a deep understanding of your patient’s very personal expectations. At the same time, it requires the ability to draw the line of professionalism especially when we are practising in a society like ours.
But what’s more beautiful than a challenge?