5 min read | Pain Science
Is tissue really the issue? : Pain Science in Physiotherapy
Written by Nirja Shah
Graphics by Kevin Thakkar
Visual Media by Param Sampat
Audio by Aparna Premraj, Natasja Azad, Param Sampat
Major Contributor: Dr. Timothy Wideman
Share this article
Peek into:
We all have stubbed our pinky toe on the table leg and sobbed in agony. Such experiences are easily explained by a structural-pathology model, which assumes that pain is an accurate indicator of the tissue state. Unfortunately, it is not that simple.
Let’s start by figuring out what happened when you first hurt yourself.
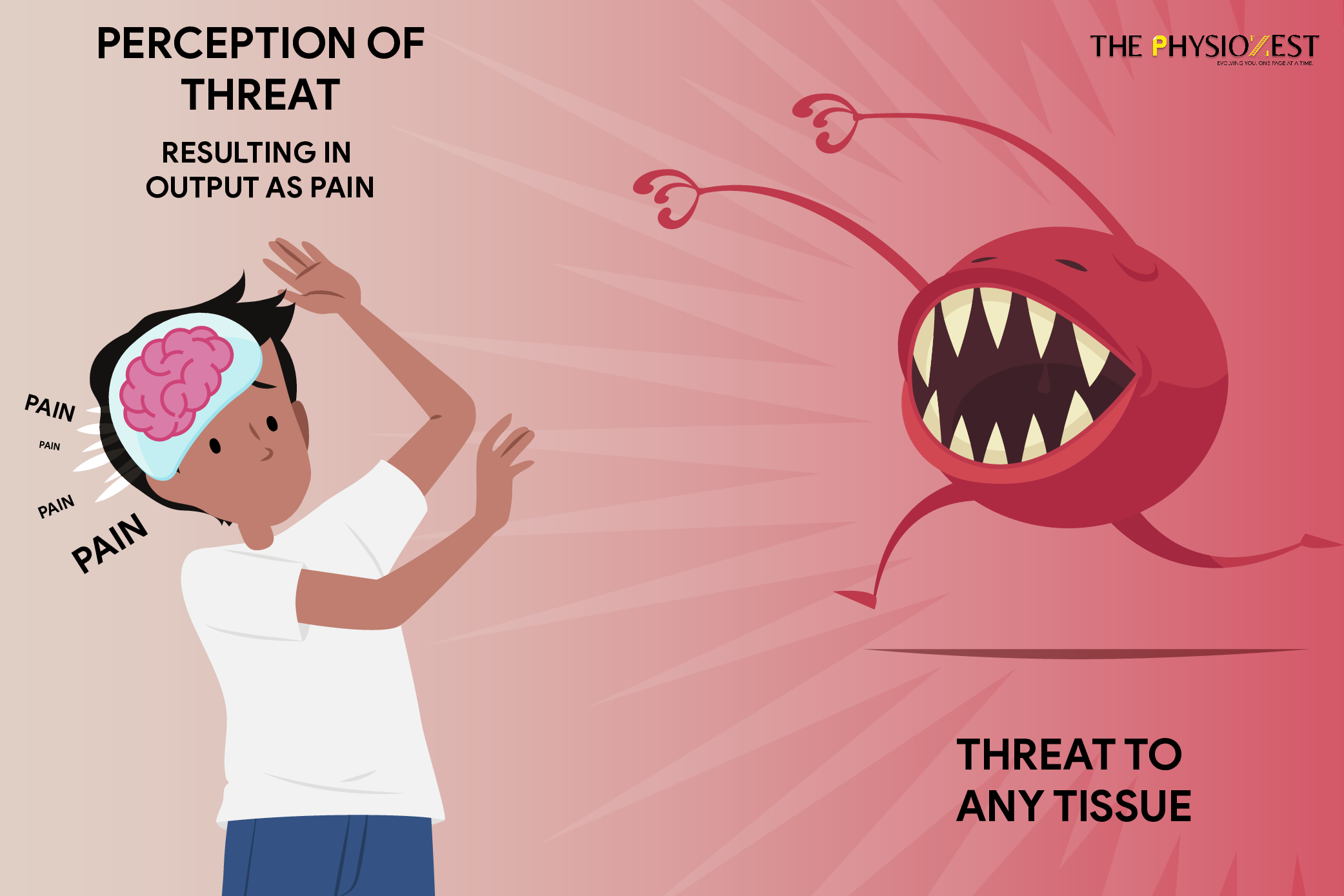
Your nerves went into a frenzy and relayed that information to your brain, which then tells you, “okay, this hurts”, but before it does so, it considers factors such as what you do for a living, your personal beliefs, whether you’ve injured your toe in the past or what you intend to do in the future! Only after you have sorted through all of this will it tell you whether or not your toe hurts. It does this extremely quickly and well before you notice anything.
In another scenario, you may experience pains that spread throughout the rest of your foot or even up your calf, far beyond the areas that were damaged. As a result, you will be forced to slow down and change your movements to avoid further injury. The nerves constantly change sensitivity in response to what is going around them and this changes the feedback that your brain will receive. It can sometimes result in significant changes in pain levels for no apparent reason.
Also Read: My Fibromyalgia Pain Story

When the nervous system is stimulated, it is common to experience pain with everyday movements such as walking, bending, or twisting. In some cases, even just thinking about a particular movement or an activity can trigger the pain.
What do you think causes this pain? We’ve all heard about Pavlov’s famous Classical Conditioning Experiment; similarly, when a person repeats a specific movement or activity regularly, the brain creates a pattern of nerve connections. The body has healed to the best of its ability, but the movement still causes pain. When a movement is painful for an extended period of time, the brain reinforces the connection between movement and pain. As a result of these connections forming, we frequently become avoidant and fearful of these movements, which strengthens the connections even more as credible evidence forms in the brain that these movements are dangerous.
Dr. Greg Lehman explains this as a pain alarm that works the same way as a fire alarm. The fire can have been put out but the alarm can keep on going. And when we have pain for a long time we can even increase the sensitivity of the alarm
All Hail the New Model
The biopsychosocial model is highly spoken about these days. There is no doubt in our minds that the transition from a pathoanatomical model of pain, to the biopsychosocial model of pain was a truly revolutionary one. Although it feels like the biopsychosocial model is new, it is not, George Engel came up with this theory in the 1970s.
“Patients, certainly, regardless of their level of education and sophistication, prefer to blame their illness on something … that happened to them and to think of disease as something apart”- George Engel
The biopsychosocial framework emphasizes three overlapping domains: biology, psychology, and society, and recognizes that processes in these three domains interact with one another to determine health, wellbeing as well as poor health, disease, and illness. That would be the model we were practicing if you took three colors of playdough pieces to represent those three different categories and started mixing them into one cohesive whole. It is about recognizing the person as a complex ecosystem rather than a bag of bones with a brain and tissues.
How to Approach Patients with Chronic Pain? Leave no stone unturned
Now that the cause has been identified, the question is – how do we apply this knowledge to our clinical practice?
The Socratic Method of Questioning is a patient-centered communication style that is widely used in cognitive behavioral therapy. It elicits and enhances motivation for behavior change by shifting the patient away from a state of indecision and uncertainty. Evidence suggests that combining the Motivational Interviewing method of Socrates with pain neuroscience is helpful for chronic pain.
Patients are wired to think of their pain as having a biological or biomechanical cause, so often the patients themselves have a more broad view of pain beneath their beliefs but only act on the more biomedical beliefs, so this type of questioning helps us overcome that and get a better idea of the root cause.
Lars Avemarie advocates the Socratic Questioning by forcing reflection and trying to explore all alternative solutions and meanings behind the pain. These meanings, metaphors, and explanations are believed to validate the patient’s own experience of pain.
There are six themes to Socrates’ questioning; this is the format you can use when framing your questions.
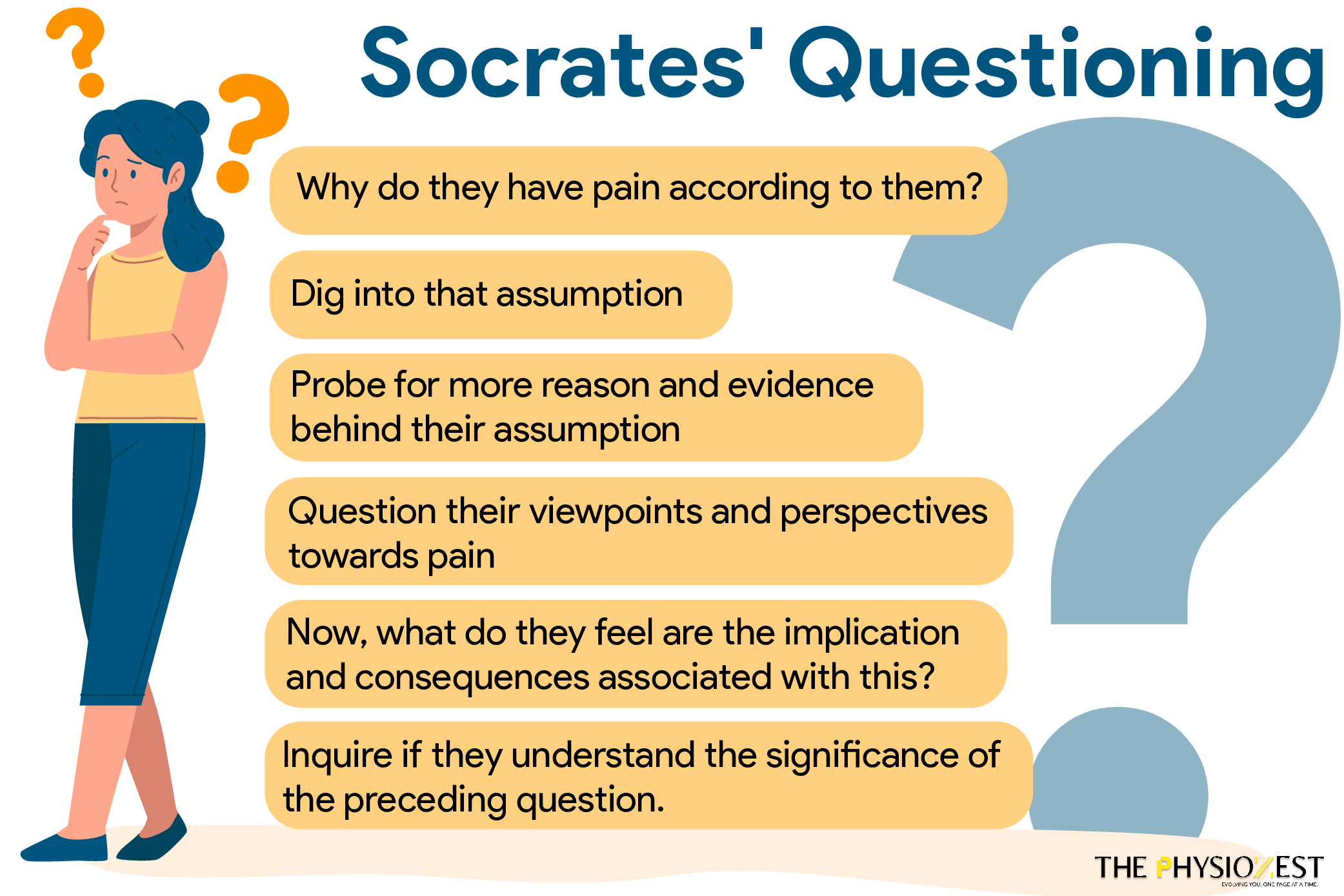
Our thoughts and perceptions frequently lead us down a predetermined path. However, these beliefs are not always consistent with what we know about pain. This type of questioning fosters good understanding and a strong therapeutic alliance, which improves cognitive and behavioral awareness and, potentially, adherence to treatment principles.
This is just the tip of the iceberg; let us delve deeper with Dr. Timothy Wideman, our pain science expert, to further integrate the subjective pain experience within research and practice.
Too bored to watch these videos? We have got you covered! Listen to the Interview on the go –