My Fibromyalgia Pain Story
Written by Janhavi Atre, Shweta Bagwe
Graphics by Kevin Thakkar
Visual Media by Param Sampat
Share this article
This is the ultimate Must Read Pain Story you should consume to identify barriers, build empathy, understand the gems of pain science and implement it in your next patient. Every Physiotherapist should read this article or save it for a future read. Sit in the chair of our character, build your Emotional Intelligence along the way!
Journal Entry– March 2018 {My Pain Story}

“We can put a man in the spaceship and send him to Mars; why can’t someone just fix this pain for me?” “Why does this hurt so badly I can’t even move?” “Will I ever be able to walk without pain?” “I’m not doing anything until all the pain goes.” Thoughts like these kept popping in my mind, and I had no answers to any of these questions. Quotes like ‘Time doesn’t heal pain; it just teaches you to live with the pain’ added to my share of existing anxiety.
Days and months kept on passing by, but the pain I was experiencing seemed to have no end. It felt like every inch of my body was crying in pain. But after reasoning, I realized that ‘Pain’ must be a word that was hated by not just me but by every other person. I decided to understand the nature of my pain and gain insight into different mechanisms of pain perception.
I could relate well to the biopsychosocial model of pain. This model categorizes the influences of pain in the biological, psychological, and social domains.
The biological contributors are bodily events. E.g., touching a hot cup of tea and withdrawing your hand after perceiving it as hot. These biological contributors activate nociceptors. Nociceptors are receptors that perceive pain.
Psychological contributors are everything else–the things we think, say, believe, predict, feel and do.
The social contributors relate to any interactions a person has with others and their roles in the social world. The amalgamation of these three categories can capture the actual state of a person’s feeling of pain.
So, I came to understand that pain is a threefold aspect.

Being an IT professional for eight years, I was expected to sit in front of a computer for a minimum of 8 hours. Also, badminton being my hobby and passion, I took an interest in practicing it on weekends and took part in interclub tournaments. Back in April 2018, at a conference in Chennai, after sustaining a severe fall from a chair, I landed on the ground on my buttocks. There was excruciating pain in my lower back region, and it became challenging for me to stand on my own, and there was numbness in my legs. There was relief for a few days after receiving PT sessions, and I resumed playing badminton. I couldn’t understand the reason for sudden pain in the neck region, and every inch in the neck and back was excruciating. While continuing my job and focussing on rehabilitation, the pain was bearable, but I had to stop playing badminton altogether. All this was frustrating!
October 2018
I had continued my job with persistent and increasing pain. MRI was (the necessity of the hour – that’s what I had perceived) done, which revealed a disc bulge in the L3–L4 region, and this made me wonder if I would have to live with this pain and ever play badminton without pain for my entire life. I started doubting my perceptions and hence decided to understand my pain profoundly.
I read about different pain models, including the biopsychosocial model, and came across a new word, ‘NEUROTAG.’ There are parts of the brain that are usually active (‘ignited’) during a pain experience.
Our brain is a network of nerves that produce output in pain perception after receiving a painful stimulus. These parts of the brain all link up to each other electrically and chemically. It’s a bit like the picture you find in the back of an airline magazine that shows all the routes across the country.
The particular pattern of activity that creates pain perception can be considered a ‘neurotag’ for pain, and the network or path that generates pain is called its neuro signature. This gave me a clear picture of my thought process, and I realized that multiple pain neurotags forming inside my brain are perceived as painful stimuli. I worked on it with my rehabilitation intensively.
My condition improved a bit but wasn’t completely pain-free.
May 2019

Having continued my job and playing badminton with persistent pain, I started feeling fatigued just after playing two games and couldn’t concentrate on my work.
She (my therapist) quoted, “All pain experiences are a normal response to what your brain thinks is a threat. The amount of pain you experience does not relate to the amount of tissue damage.” It was explained that every person perceives pain differently. Some of my symptoms, mainly pain in muscles accompanied by fatigue, tiredness, and anxiety, were among the chief complaints of fibromyalgia. She said that the pain experience of the brain relies on many sensory cues.
Our brain is a multitasker. Therefore, a single cell can produce multiple neurotags for pain, leading to a perception of chronic pain.
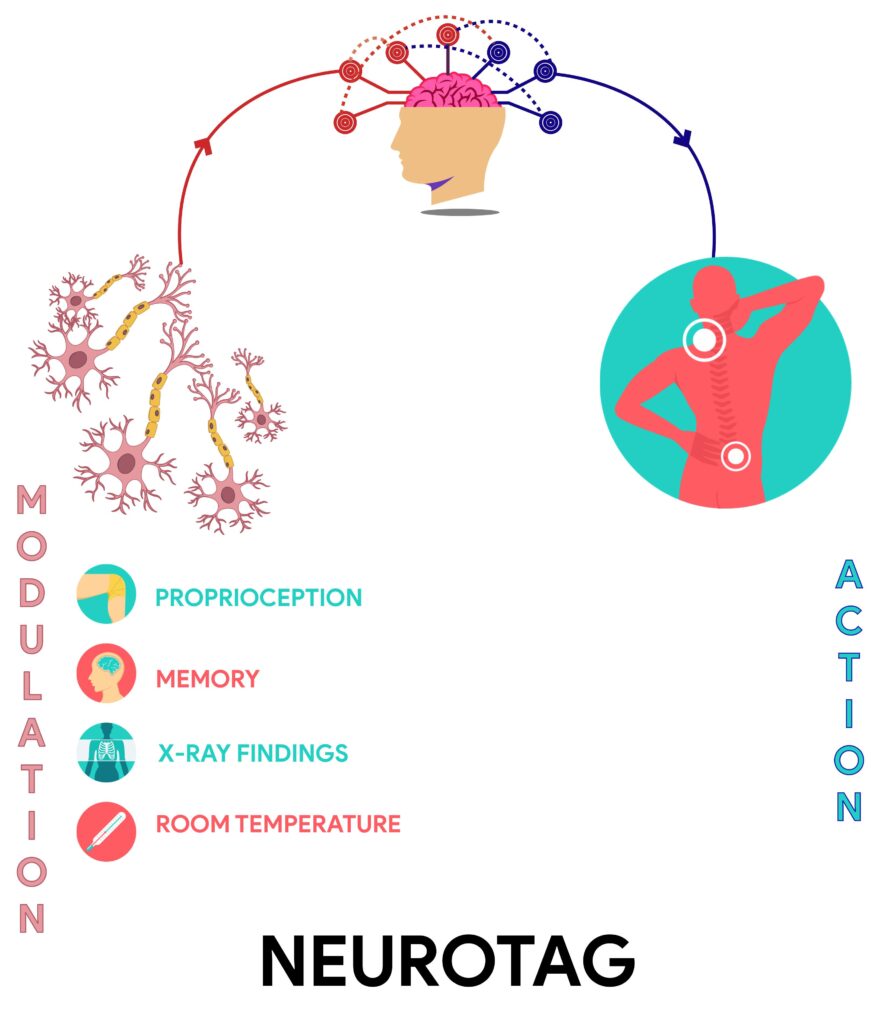
Pain or nociception neurotags activate a vast network of brain cells. When pain persists for a long time, pain neurotag becomes more significant in size and shape, increasing its mass and increasing pain perception.
To overcome this perception, she introduced a TARGET CONCEPT for pain management. Catchy slogans like “Motion is lotion,” “Movement is the key to recovery,” and “Don’t flare up,” “But don’t freak out if you do” resided on my fridge instead of fridge magnets and also on my office board. Practicing these slogans seemed to increase the influence of the newly formed neurotags and reducing the impact of pain neurotags which modulated my reducing pain perception.
November 2019 {My Pain Story}
In fibromyalgia, the pain seems to result from neurochemical imbalances in the central nervous system, leading to a “central amplification” by increasing sensitivity for pain perception. She explained this concept of chronic pain by giving a simple example- a computer malfunction. One keystroke on the keyboard (the tissues), such as ‘substance’ P (in the tissues), creates many P’s on the computer screen (spinal cord).
This is how pain amplifies, and the brain becomes increasingly sensitive to it. This increased sensitivity should fade once the damaged structures are under control and fully understand what is going on. If you had a nasty accident on a street corner, every time you pass that area, you might have a reminder, perhaps just a shudder, a pain neurotag is constructed in your brain.
Your brain is looking out for you.
The more chronic the pain becomes, the more complex the changes in the brain become. These changes are strategies by which the brain ‘looks out’ for you–by making the body part challenging to use (smudging of motor areas in the brain) or making nearby body parts sensitive (smudging of sensory regions in the brain).
It is reversible.
Just like how muscles and joints can be made more healthy, so too can the homuncular arrangements in your brain.
December 2019
As my rehabilitation progressed and my perspective about pain changed, I felt more positive about my progress towards pain relief. My therapist tried explaining a new concept of identifying DIMS (Danger in Me) and SIMS (Safety in Me). A DIM is a ‘danger in me’ message which relates to the things you do, the people in your life, places you go, things you think and believe, something you say, and things you hear, see, smell, taste, and touch.
My DIMS & SIMS

After understanding the psychology of pain from my therapist, my perspective about pain changed, and the pain was no longer a problem.
January 2020
My pain threshold has increased. Pain threshold refers to the minimum intensity at which pain is experienced.
Now I could sit without pain for 3 hours continuously. My physiotherapist introduced different ways of performing a particular exercise if one way failed and induced pain and provided me with varying backup plans for pain management (Brain redundancy).
For further read-
Books- Explain Pain & Explain Pain Supercharged
Research Paper- Redundancy in synaptic connections enables neurons to learn optimally
I endured playing five games of badminton and took part in interclub tournaments, and that too WITHOUT PAIN.
We all know that pain is a very complex and subjective term. Getting out of pain is never easy in the first place.
What did I follow?
- Identify and eliminate as many DIMS as you can.
- Identify & incorporate as many SIMS as you can.
- Understand the concept of Neurotags and create Target Neurotags.
- Do not overburden your body if it cannot take the pressure.
- Understand Brain Redundancy.
- Graded exposure to exercise works best for CHRONIC PAIN.
TURN YOUR PAIN INTO POWER AND CONQUER GOALS
Contributors

SHWETA BAGWE
Research & Content Writing Team
JANHAVI ATRE
Research & Content Writing Team
PARAM SAMPAT
Multimedia Team

KEVIN THAKKAR
Multimedia Team