9 min read | Physical Therapy Rehab
Meniscus Repair Rehabilitation: Aggressive Or Non-Aggressive Route
Written by Maria Dalal, Rutvi Shah, Shweta Bagwe
Graphics by Pranali Oswal
Audio by Nidhi Joshi, Natasja Azad
Share this article
Table of Contents
“Two roads diverged in the woods
And I took the oneThat had better scientific backing
Applied to my client’s specific needsAnd that has made all the difference
-ROBERT FROST (PT)
Meniscus injury rehabilitation scares me, I’ll admit.
Nobody agrees about which road to take- should we restrict the range and go non-weight bearing?
Or will the repair benefit from weight-bearing immediately?
When confused, we put our faith in evidence-based perspectives.
Join us on a comprehensive study of the latest literature available and make an informed decision.
Menisci are the C shaped fibro-cartilaginous structures on the tibial plateau that:
The most common mechanism of injury to the menisci is a twisting injury with the foot anchored on the ground and knee flexed, often due to contact with another player’s body. Tear length, tear depth, and tear pattern affect the type of repair and ensuing recovery.
What is the GOAL of Meniscal repair?
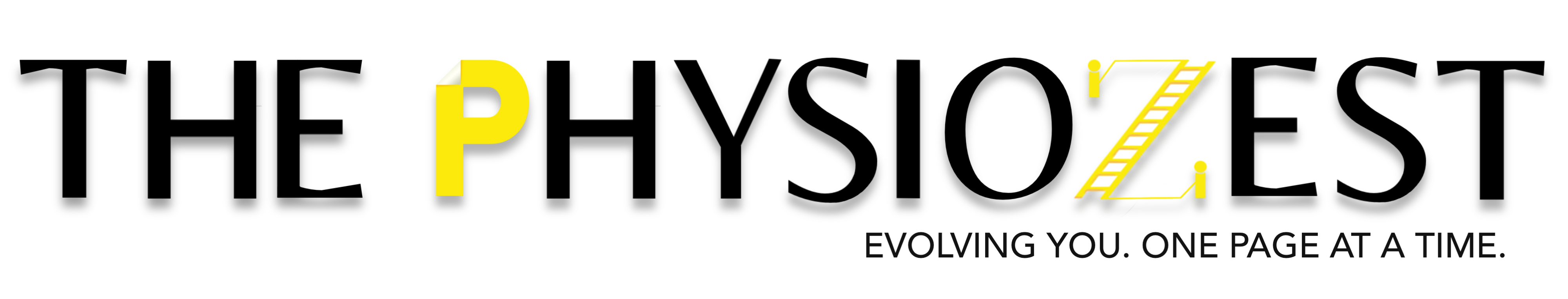
Types of Repair
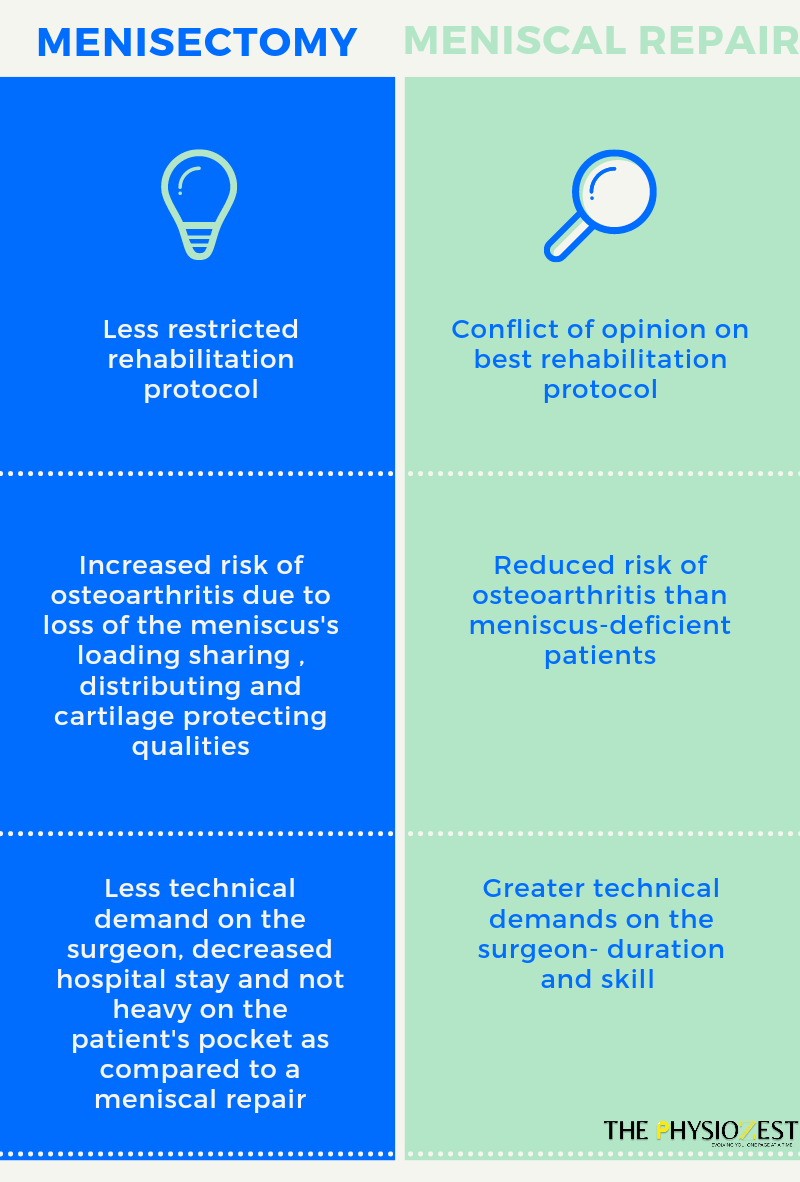
Healing after meniscus repair depends on
Aggressive VS Non-aggressive Rehabilitation

Yell at the meniscus till it starts doing its job, the little slacker. Dosage: 2-3 hours a day, 7 days a week.
Aggressive vs non-aggressive rehab has no strict distinction and offers a range of protocols. However, most studies agree that limiting the range of motion and weight-bearing before 6 weeks is considered Traditional Non-Aggressive. An early weight-bearing and tolerated range of motion in the immediate postoperative period is considered an Aggressive or Accelerated Approach.
The goal after the repair is to protect the surgical repair while balancing the costs of immobilization and disuse. The location, size, vascularity, and repair technique play a major role in outcomes. Concurrent injuries, apprehension or recklessness towards the return to sport, and the mental health of the client are top priorities.
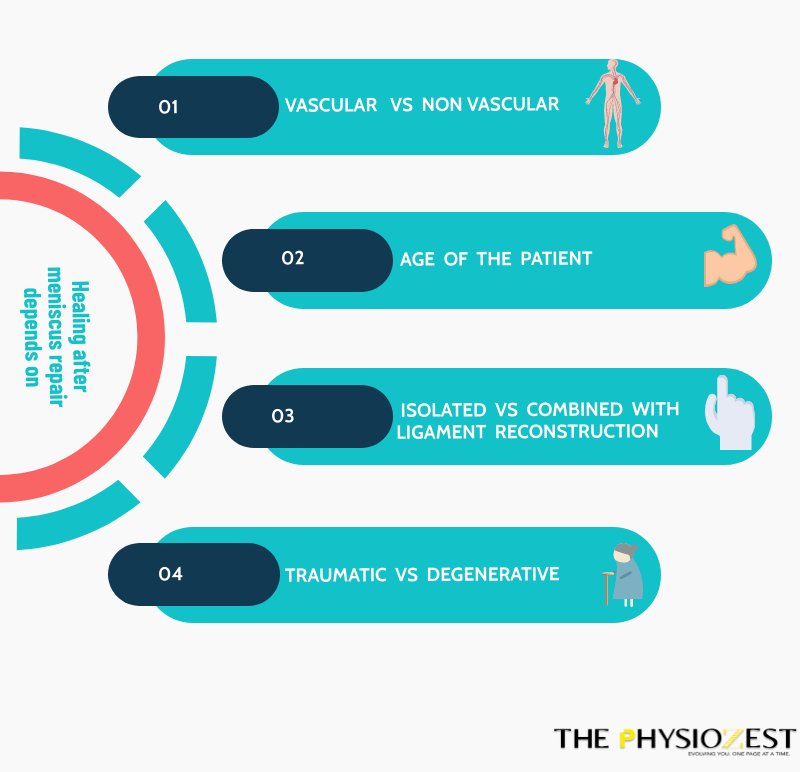
Non-accelerated Rehabilitation
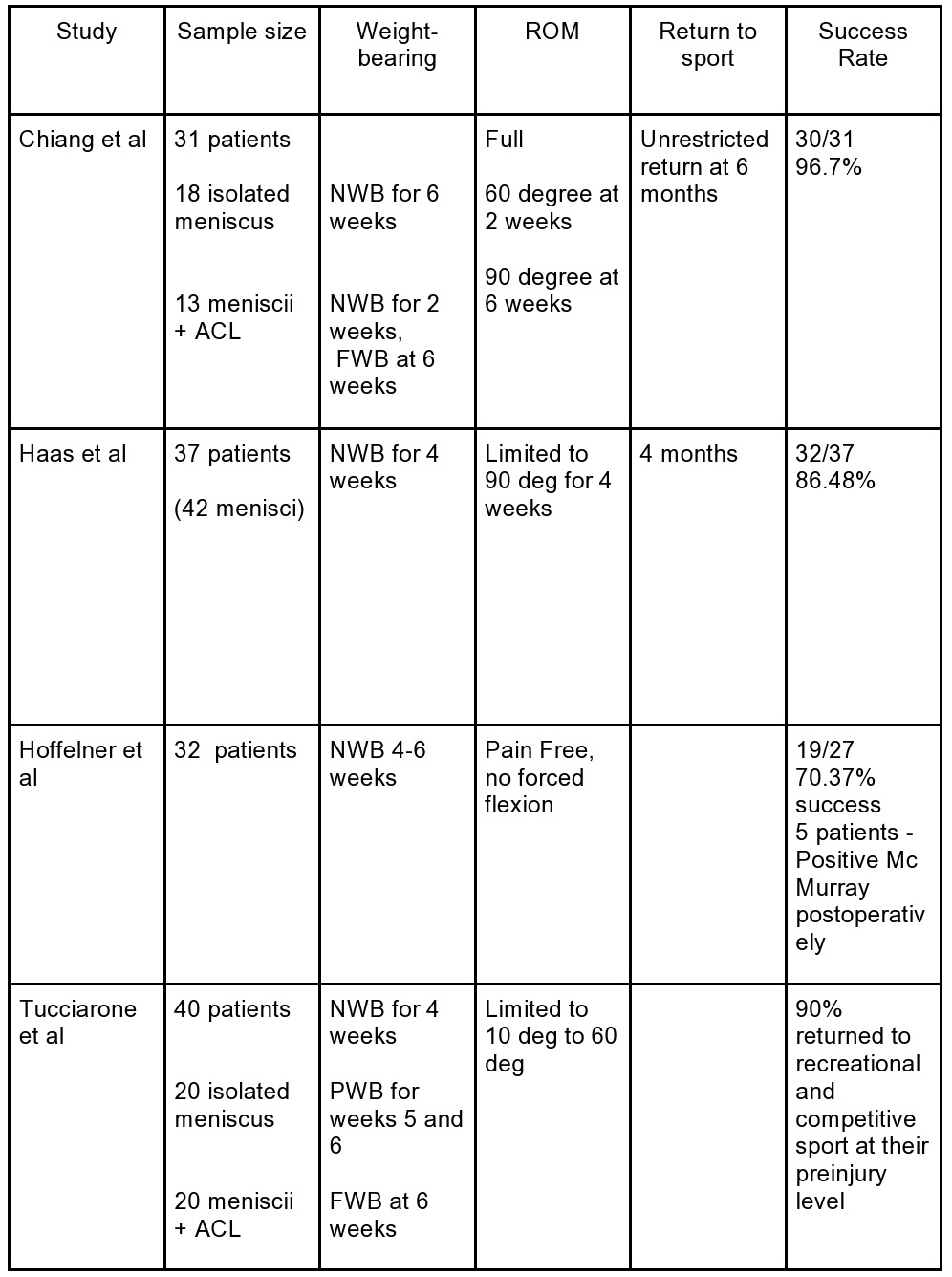
Table 1: Summary of the studies undertaking Non-accelerated rehabilitation after Meniscal Repair surgery, with sample size, Weight-bearing instructions, Range of motion allowances, and the success rate of rehabilitation [1]
Accelerated rehabilitation
The core principle of this form of rehab after the repair is:
“ Simultaneous Protection And Progression”
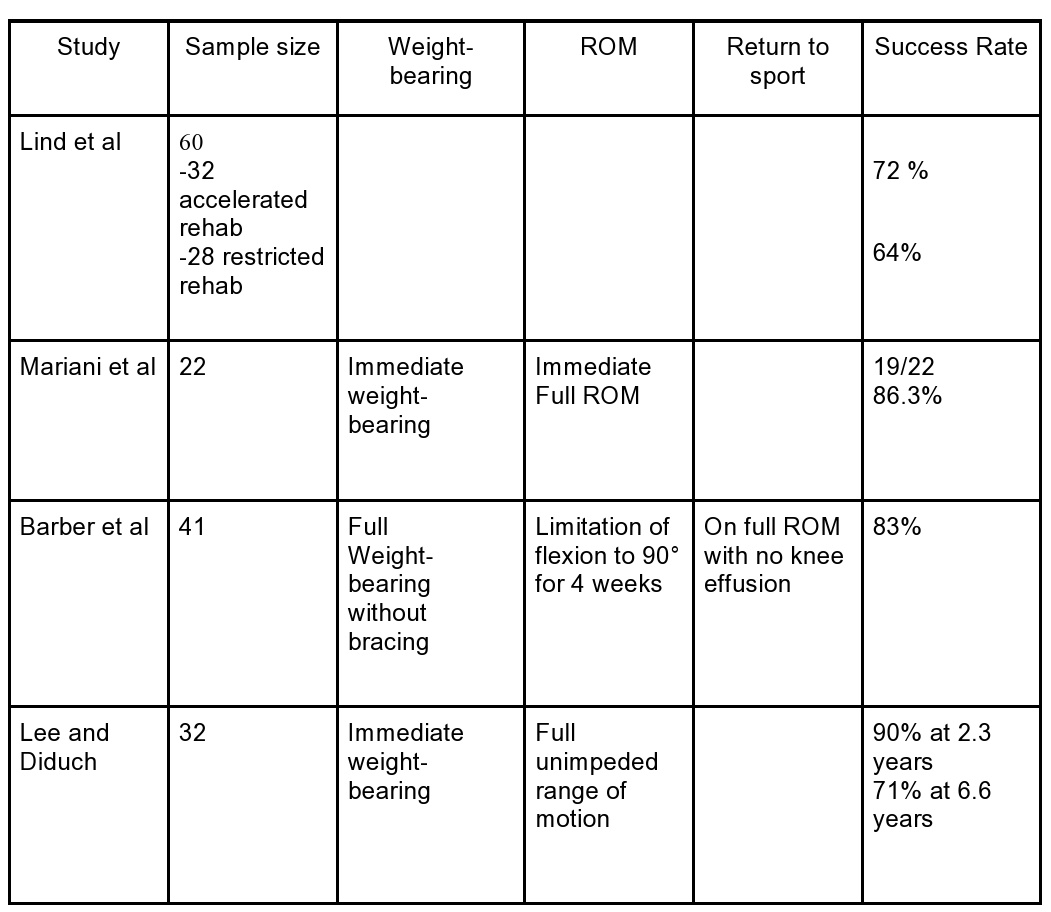
Table 2: Summary of the studies undertaking Accelerated rehabilitation after Meniscal Repair surgery, with sample size, Weight-bearing instructions, Range of motion allowances and the Success rate of rehabilitation [1]
Successful clinical outcomes ranged from 70% to 94% in the studies reviewed here. More recent studies have tended toward an accelerated rehabilitation protocol with full weight-bearing and early range of motion. Reported outcomes in the studies reviewed are comparable (64% to 96% good results) to the more conservative protocols.
Multiple events were considered as failures of rehabilitation in the above studies, which include anatomical retears, return of symptoms (pain, knee effusion, clicking), and positive Mc Murray’s sign-on follow up.
An additional advantage that accelerated rehab has over its traditional counterpart is a sense of control over the demoralizing period of recovery, from the patient’s perspective
“Consensus on Census- Which population benefits most from Accelerated Protocols?”
Young individuals who want to return to High-Performance Sports are the beneficiaries of an accelerated protocol.
Return-to-Sport Rehabilitation Progression Principles:
Return-to-play criteria
Conclusion
The recovery of meniscus injury is multifaceted- with factors like location of the tear, pattern, vascularity, surgical technique, and age, various influencers of mental health, attitude towards recovery, coaching, and support system impacting the healing process. Like any injury, the best chances of success come when we approach not just the knee, but the person.