6 min read | Physical Therapy Rehab
Bell’s Palsy: Getting on your Nerves?
Written by Aditi Parekh
Graphics by Nimisha More
Visual Media by Pooja Chetwani
Audio by Chinmayee Patil
Guest Contributor: Dr. Meghana Dave
Share this article
Table of Contents

All that Palsies is not Bells.
Everyone has come across patients suffering from Bell’s palsy which not only affects physical functioning but affective domains of their life.
The first thing that needs to be understood is the onset of the condition and the cause. People who have a history of a past viral infection including COVID are at a higher risk. This information helps us in understanding the prognosis. Secondly, it needs to be considered whether the patient has had steroid medications within 72 hours of onset (to reduce the pressure and swelling around the nerve), this helps in faster recovery. The differential diagnosis that affects the facial muscles such as stroke, brain tumor, injury to the ear needs to be ruled out before formulating the plan of care.
Today, Dr. Google diagnoses most of the patients before us and guides them through specific treatment protocols.
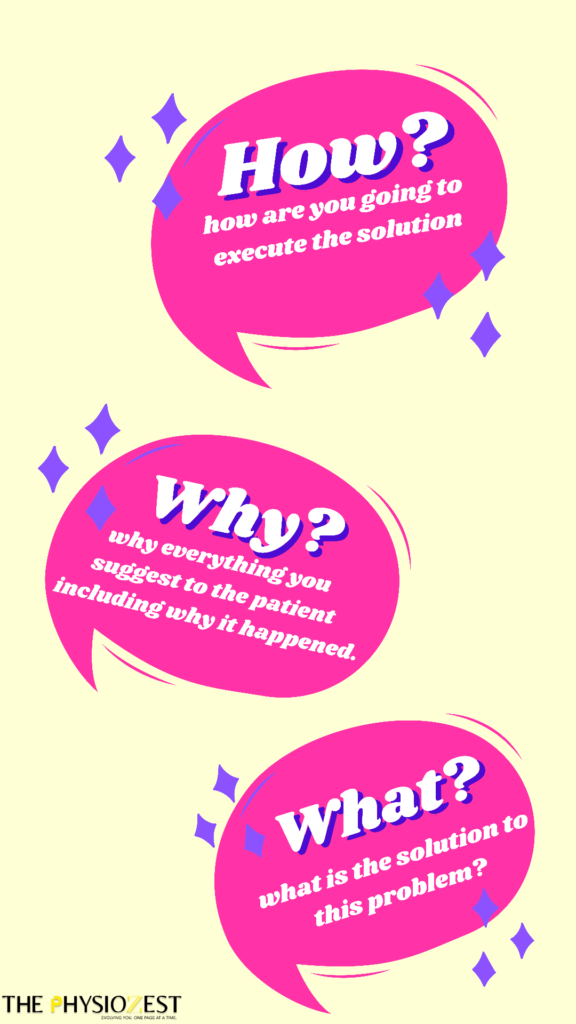
Rational Communication
Electrical Stimulation in Facial Palsy: Is it History yet?
Electrical Stimulation is one of the first things we learn in our clinical rotations. It’s less time-consuming and effective!
It has been in use since around 1975 and yet continues to be the sole treatment choice of many practitioners, albeit without any concrete research.
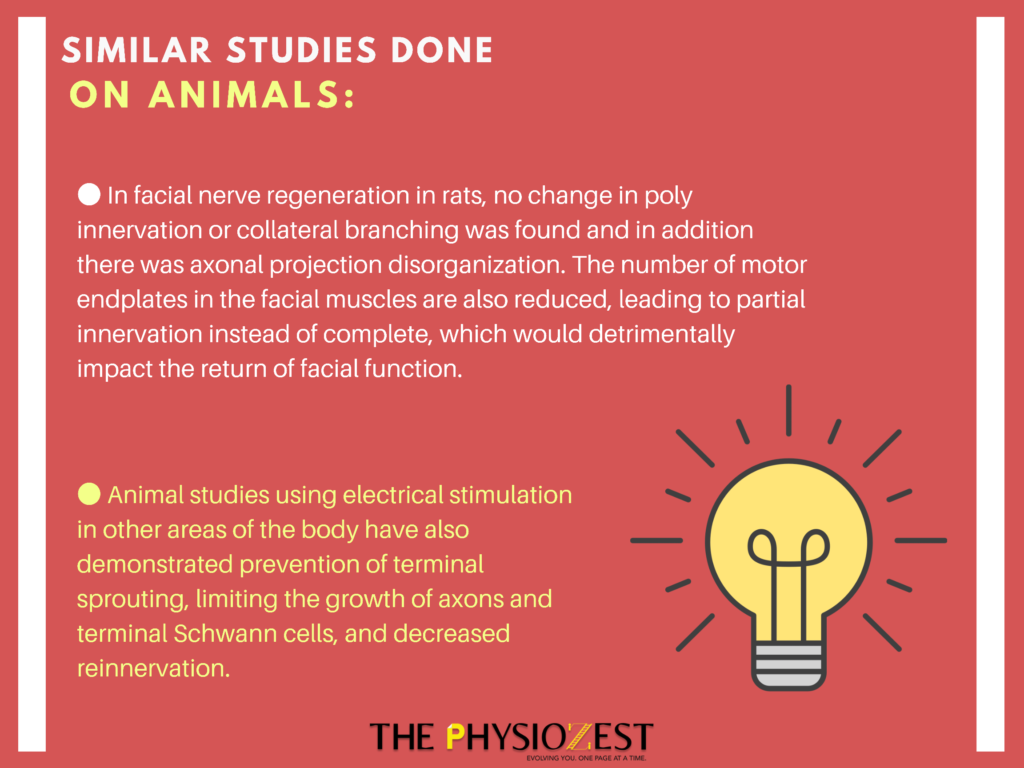
Even though it seems to be working, studies have concluded that Electrotherapy may be unnecessary and indeed contraindicated for most of the patients.
Why?
Lack of observed movement in facial palsy is mainly due to abnormal synchronization and the contractions produced by electrical stimulation may activate overactive muscles reinforcing abnormal patterns.
The core in the treatment of synkinesis (i.e voluntary contraction of one muscle causing involuntary movement in other muscles) is to inhibit abnormally contracting muscles as opposed to facilitating flaccid ones.
Research suggests that electrical stimulation does not alter the speed or rate of recovery, nor does it improve facial function in the acute phase. In the chronic phase of recovery, evidence about extensive electrical stimulation having a positive impact on facial function is extremely low.
Neuroplasticity: A Bane or a Boon?
Book recommendation- ‘The Brain that Changes itself’ by Norman Doidge.
What other options should we look at then?
1. Mime Therapy
Mime therapy refers to the treatment in which therapists utilize emotional input to access better movement patterns. For example, as the patient practices their balanced smile, they encourage patients to think of something that makes them happy. The aim of mime treatment is to promote symmetry of the face at rest and during movement; the patient is being simultaneously taught to control synkinesis. This will result in reduced stiffness and increased emotional readability.
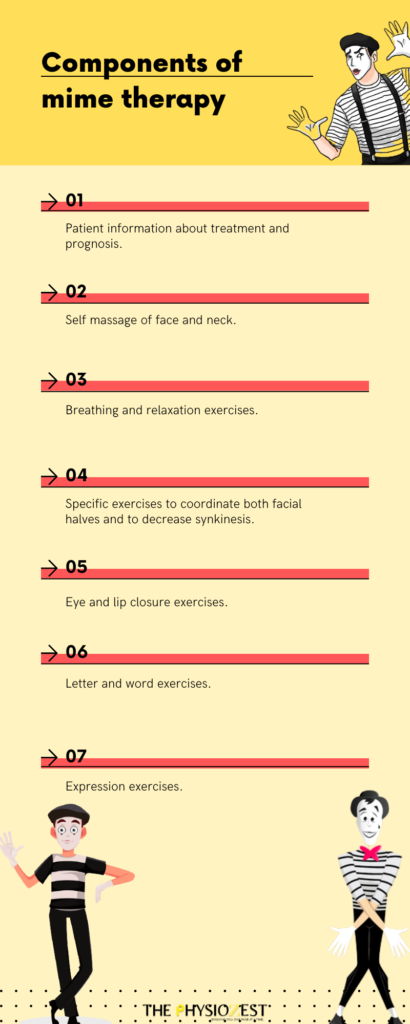
The facial appearance, functional status, and outcome measure scores have shown improvement in patients after mime therapy.
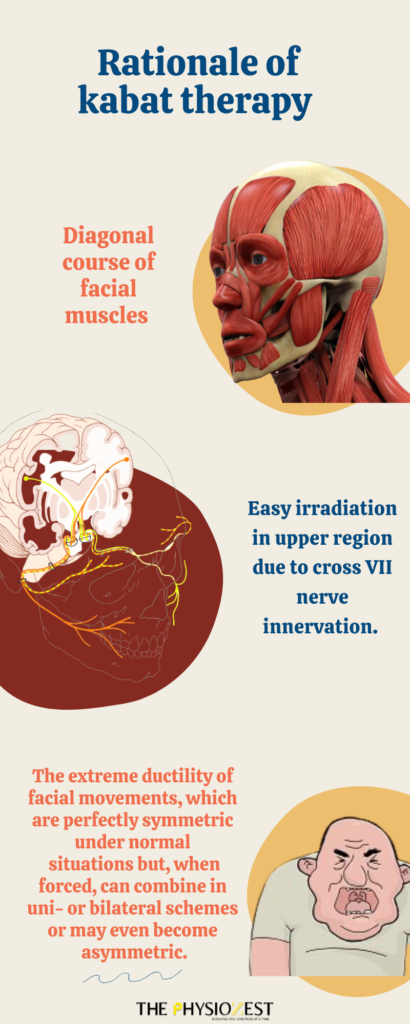
2. Kabat Therapy
This method is based on proprioceptive neuromuscular facilitation which considers harmony, coordination, and optimal strength of body movements. It majorly depends upon the concept, of diagonal lines with respect to the sagittal axis of the body, thus implying a ‘‘rotational’’ effect and facilitation of voluntary response of an impaired muscle through a global pattern of an entire muscular section
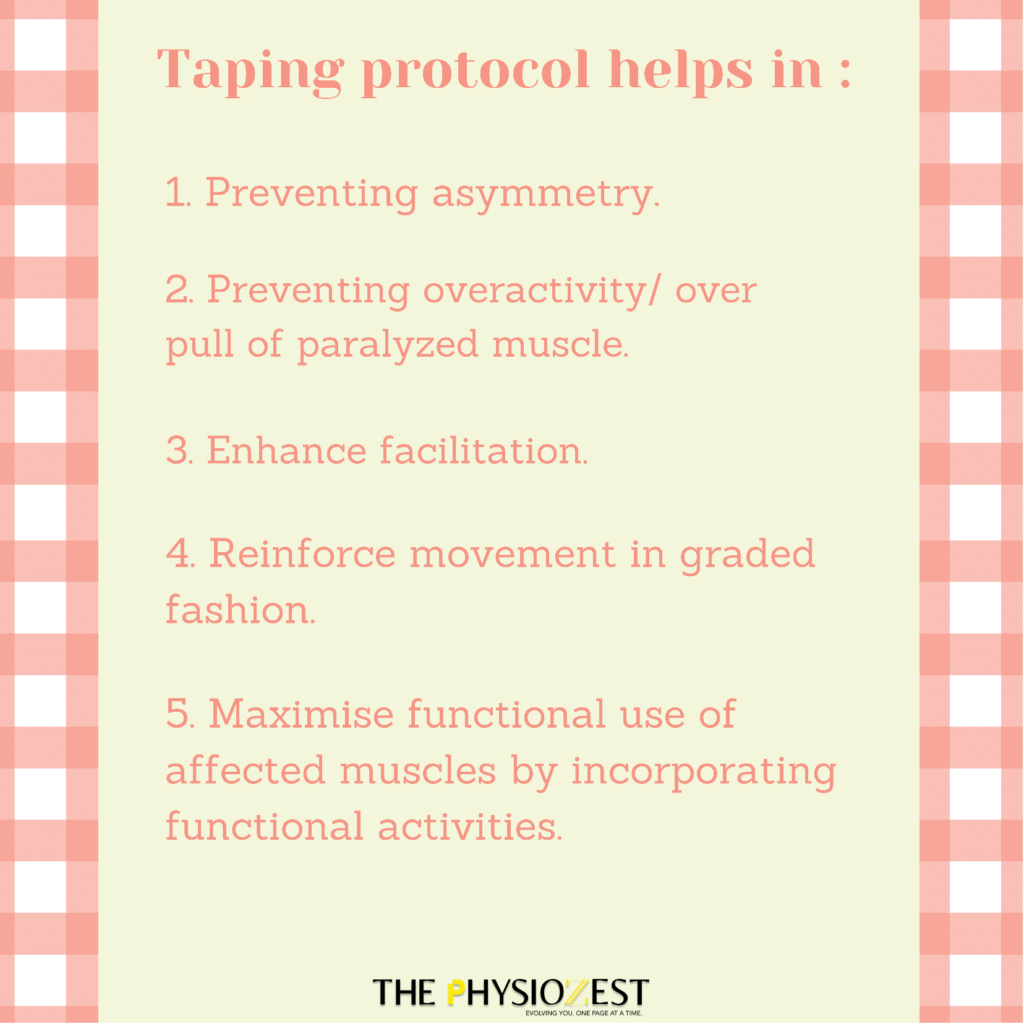
3. K Taping
Taping helps to retrain paralyzed facial muscles by maintaining symmetry and facilitating paralyzed muscles, thereby preventing over activity of normal muscles, and acts as a stabilizing mechanism by promoting desired symmetrical movement pattern that needs to be repetitively reinforced before it will be learned.
It works on the principle that weak or paralyzed muscles can be reinforced or facilitated through irradiation and temporal/ spatial summation.
4. Motor Imagery and Mirror Therapy

Points to consider before starting a treatment protocol.
In the future, when a patient comes to us with a physician’s reference stating “To physiotherapist, please give electrical stimulation to this patient for bells palsy,” let’s take a minute to think over the fact before blindly following the instructions and dive in deep to the specific etiology of your patient.