6 Red Flags you need to watch out for while Treating Back Pain
Nirja Shah | 4.9 min read | August 3rd, 2021
Share this article
When was the last time you labeled a patient as a Chronic Low Back Pain Case OR diagnosed the patient as Para Spinal Muscle Spasm (PSMS)?
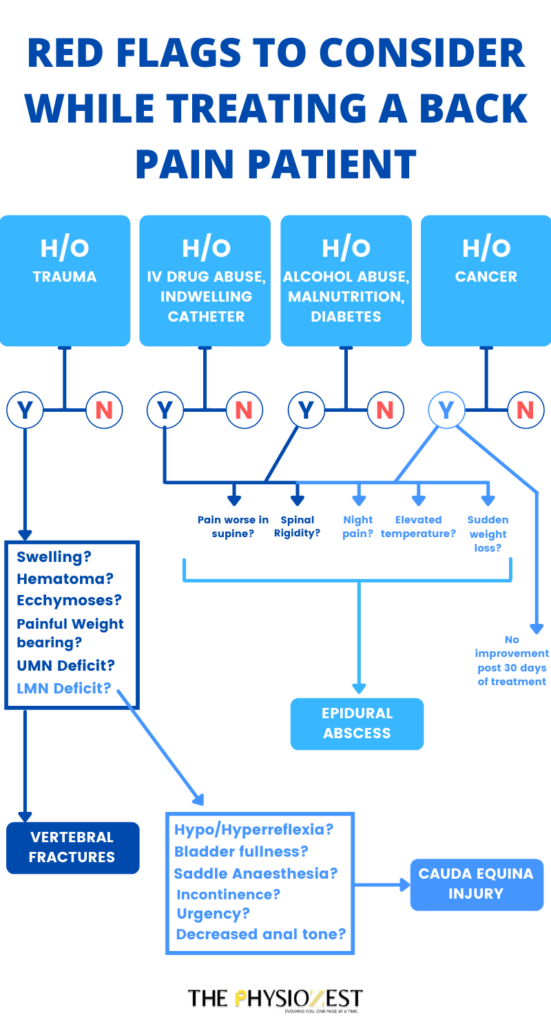
Well, we are constantly under threat to overlook small red flags and surrender to the monotony. With limited access to perform investigations in primary care settings, it might be extremely challenging to distinguish between innocent symptoms and serious medical conditions. For each presentation, we look for red flags that are clinical indicators of possible underlying severe conditions requiring further medical intervention.
This list will save you from surrendering to monotony and start actively ruling out the probable etiology for Low Back Pain.
1. Age isn’t just a number
Patients above the age of 50 are considered to be at risk for vertebral fractures.
2. Constant pain with no change in VAS during activity
Recently a runner came up to the clinic with mid-thoracic vertebral pain. It looked like a general runner’s back pain complaint due to reduced thoracic mobility. But the tables turned when we asked him about VAS on rest and activity; they were the same! The usual line of treatment protocol might have been to use an electrical modality, exercise prescription, and patient education. But that would have been dangerous for him. Think about the answer until you reach the explanation below!
3. Falls, literally (not for people)
Significant trauma events like vehicular accident, fall from a height, or direct blow to the spine put the patients at risk for developing vertebral fractures.
Do they have pain with weight-bearing.
Back tenderness.
Altered temperature.
Muscle spasm.
These are some of the questions physiotherapists should note while examining a patient with back pain. You might even notice some swelling, hematoma, or ecchymosis along the suspected area of pain. If the trauma has caused injury to the cauda equina or nerve roots, the patient might show signs of upper motor neuron or lower motor neuron deficits.
4. Fever, chills & spinal rigidity leading to reduced accessory mobility
Does your patient complain of sudden fever, chills, and unexplained weight loss along with a history of IV drug abuse or an indwelling catheter? They might have a spinal infection or an epidural abscess. These patients are seen to have spinal rigidity leading to reduced accessory mobility.
5. Unexplained weight loss
Patients with a history of prostate, breast, lung, or other cancers might present with progressive back pain over several months along with night pain or pain at rest. This should trigger clinical suspicion, especially if the patient has had unexplained weight loss over the past few months. These patients usually show no improvement after 30 days of treatment, which warrants additional diagnostic studies.
Runner Answer: The runner had been diagnosed with a neoplastic lesion in his vertebrae (CT Scan), and neither a heating modality nor patient education would have helped him.
6. Bladder or Suprapubic fullness
If the patient complains of bladder or suprapubic fullness and numbness along with the anus, perineum, and genitals, there is a possibility of cauda equina compression causing back pain. Your patient also might report urinary retention, increased frequency, or overflow incontinence. They might also have decreased anal tone leading to fecal incontinence. On examination of their sensations and reflexes, you might discover hyporeflexia or hyperreflexia along with loss of light touch and pinprick sensations. It can suggest spinal compression, and additional evaluation needs to be performed for these patients. You might observe progressive neurological deficit in the form of knee extension weakness and foot drop.
The use of these red flags could help physiotherapists avoid over-reliance on diagnostic tests and provide early intervention for patients with back pain so they can get back up on their feet in no time.
References:
- Galliker G, Scherer DE, Trippolini MA, Rasmussen-Barr E, LoMartire R, Wertli MM. Low back pain in the emergency department: Prevalence of serious spinal pathologies and diagnostic accuracy of red flags. Am J Med. 2020;133(1):60-72.e14.
- Downie A, Williams CM, Henschke N, Hancock MJ, Ostelo RWJG, de Vet HCW, et al. Red flags to screen for malignancy and fracture in patients with low back pain: systematic review. BMJ. 2013;347(dec11 1):f7095.
- DePalma MG. Red flags of low back pain. JAAPA. 2020;33(8):8–11.
- Villacorta J, Kortebein P. Peripheral arterial disease masquerading as low back pain. Am J Phys Med Rehabil. 2012;91(12):1104–5.
- Delitto A, George SZ, Van Dillen L, Whitman JM, Sowa G, Shekelle P, et al. Low back pain: Clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American physical therapy association. J Orthop Sports Phys Ther. 2012;42(4):A1–57.